Cardiac Risk Calculation
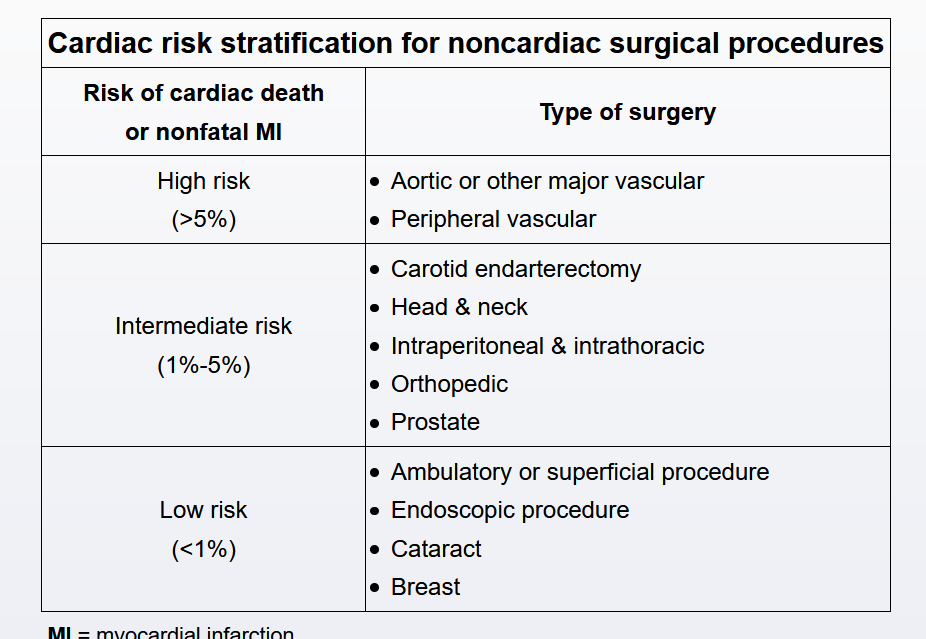
Determining perioperative cardiovascular risk requires consideration of the type of surgery being performed as well as the clinical comorbidities and functional status of the patient. The level of risk associated with the particular noncardiac surgery should be considered first; patients undergoing low-risk surgeries (eg, breast or cataract surgery) have <1% risk of experiencing cardiac death or nonfatal myocardial infarction (MI). In the absence of acutely active cardiac disease (eg, decompensated heart failure, unstable angina), patients undergoing these low-risk surgeries require no further cardiac workup regardless of underlying comorbidities.
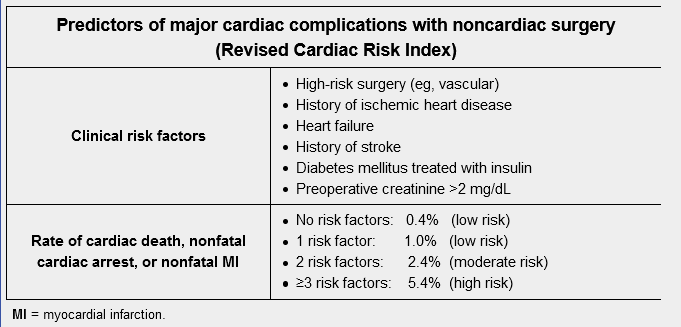
For intermediate- or high-risk surgeries, patients should be evaluated using a validated prediction model such as the Revised Cardiac Risk Index (RCRI). Moderate- or high-risk patients (ie, with an estimated risk of cardiac death, nonfatal cardiac arrest, or nonfatal MI >1%) may need additional evaluation depending on their functional status: Those able to perform >4 metabolic equivalents (METs) of activity (eg, brisk walking, climbing 2 flights of stairs) generally do not require additional evaluation, but those with poor functional status (exercise capacity <4 METs) are recommended to undergo further evaluation prior to surgery.